Thank you for your help for my recent operation.
Here is a copy of the email to enlighten you as to why I was so particular about the anesthesia to be used.
Start at the very bottom of this document to see my original email to Dr. Friedberg. His reply explains why I only wanted to use propofol.
Take a peek at his book, ‘Getting Over Going Under’ (free from his new website www.goldilocksfoundation.org) It explains a lot about what a patient needs to know about anesthesia, especially if they are over 50 and going to have an operation that requires sedation during an operation.
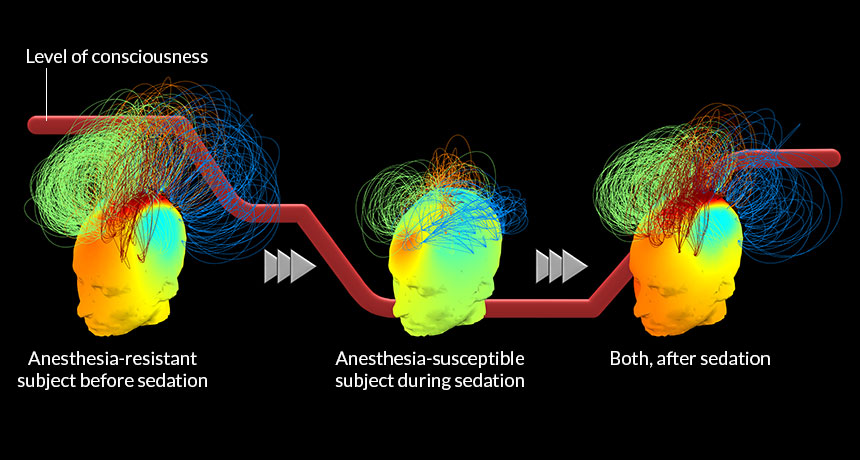
The book will also explain why anesthesiologists don’t take the simple route for smaller operations like cataracts or cosmetic surgery. But, they should be using a BIS Brain Monitor for larger operations and most patients would not know to even ask about this. This meter can avoid the problems associated with being over-medicated with anesthesia.
By requesting “NO BENZOS” I had NO PAIN, NO NA– USEA, NO HEADACHES, NO FATIGUE, NO PROBLEMS. Propofol was used and just put me to sleep. When I awoke, I was in the recovery area and was wide awake and alert. We went for breakfast and then I went to work. I was PAIN-FREE, not tired, not drowsy, not sleepy, not dizzy; BUT, I had to demand it, otherwise, the anesthesiologist would have given me the usual cocktail of benzo-type ( benzodiazepines) drugs.
Feel free to forward this information to anyone you know that may be getting ready for surgery.
Have a nice Thanksgiving.
Dan
My response:
First, let me sympathize with your wife’s condition & extend my fervent wish that I could offer something to reverse it. Sadly, I cannot.
Second, your cataract surgery is so short that it would not be of any benefit to have the BIS brain monitor.
PUBLIC EDUCATION MESSAGE: NO MAJOR SURGERY UNDER ANESTHESIA WITHOUT A BRAIN MONITOR
Your cataract surgery, while major in your eyes, is not ‘major’ surgery.
Next, the only thing I would tell your anesthesiologist is ‘no benzodiazepines please.’ Just a little propofol for sedation would be great.
Lastly, after MUCH frustration with my colleagues’ reticence to adopt this monitor, I created this following in a fit of despair…& created this…
Here is my book you requested… I wrote it in plain English for the general public to help deal with anesthesia fears…
virus free
I need your assistance.
The best thing you can do with my book after reading it is sharing it with as many of your friends & family members, especially those over 50, as you can.
I cannot access those people myself & they might not perceive such a contact from me as welcome.
The reason for my non-profit foundation (& disclaimer) is to avoid any suspicion that I am somehow making money by my advocacy.
Dan’s original email
Dear Dr. Friedberg,
My wife had 3 lumpectomies and a mastectomy within 4 months. (About 5 years prior to these operations, she had a heart valve replaced.) She has developed dementia/ Alzheimer’s since the mastectomy.
I am about to have cataract surgery and would like to obtain a copy of your book: ‘Getting Over Going Under, 5 things you MUST know before anesthesia.’ Will your advice apply to the anesthesiologist for cataract surgery?
I had cataract surgery on my other eye about 2 years ago. When I began to question the anesthesiologist, he was very put out and abrupt with any answers. His attitude was about doing his job for 20+ years and he knew what he was doing. I want to be ahead of the curve this time around—scheduled for 11/19.
If I am told they don’t have a brain monitor at the surgery center (not in a hospital), is this something that can be readily obtained, borrowed or purchased? And, if they don’t have the equipment, is it likely that the doctor would be trained in how to use it?
Thank you in advance for any guidance.